- 6
- 3
Done:
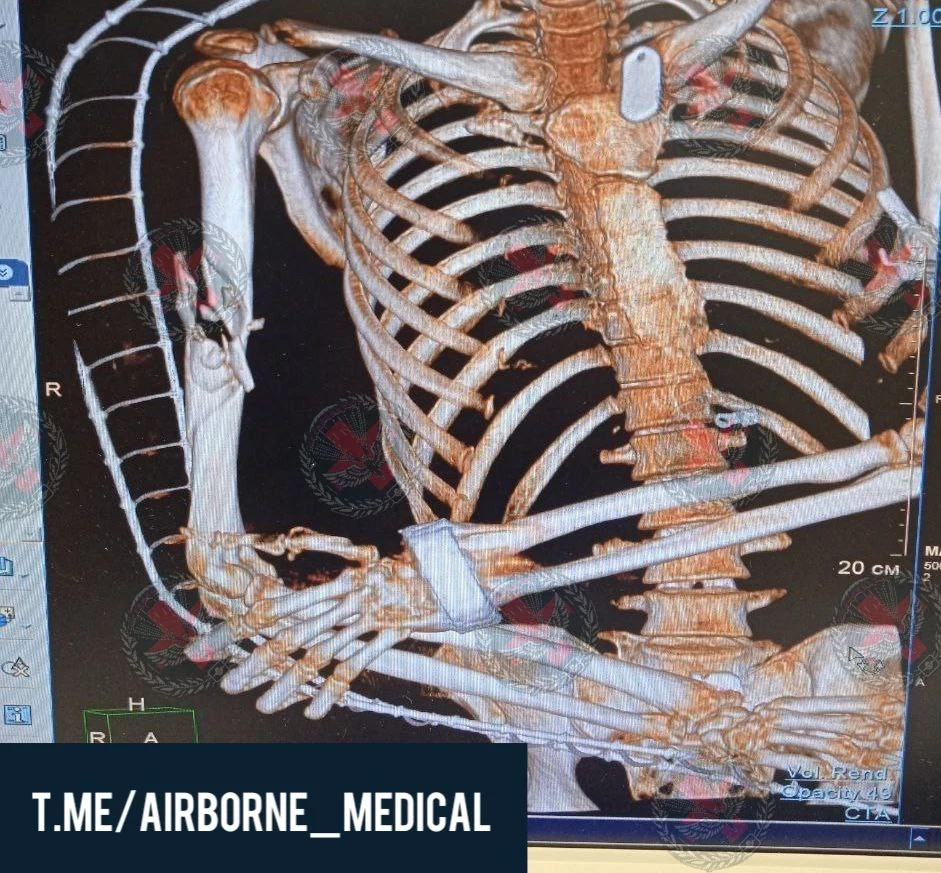
Anterolateral thoracotomy on the right.
Opening the pericardium and suturing the wound of the right appendage. Suturing wounds of the right lung. Sanitation and drainage of the right pleural cavity. Dressing wounds.
(I posted it before I'll provide link later because it's midnight in my place rn, it's continuation of previous post)
- 1
- 3
- 4
- 11
From a safety point of view, this isn't scary, since inside such an implant is a saline solution that isn't harmful to the body.
- 3
- 13
Genitalia are a key element for male self-esteem, contributing towards mental and physical balance and influencing their social life [2]. The Authors confirm that the most frequent cause of penile skin loss is trauma. Tumors, infection and iatrogenic causes are also reported in the literature. In a previous paper of this journal we presented a case of iatrogenic skin shaft sub-amputation of a 27-years old HIV positive man, after a catastrophic circumcision procedure, repaired with a scrotal dartos-fascio-myo-cutaneous flap [3]. Skin graft represents the most popular and simplest reconstructive procedure and H. Aineskog et al. presented a very suitable case. Nevertheless, we reckon that skin graft provides poor tissue elasticity with less resistance to sexual intercourse and higher risk of retraction than free o local flaps [4]. Scrotal dartos – fascia – myo-cutaneous flaps were harvested on both the lateral parts of the scrotum (Fig. 1) and the donor site was easily closed for primary intention using cutaneous non absorbable interrupted sutures. Anterior scrotal vessels and nerves supply the flaps.
Scrotal dartos-fascio-mio-cutaneous flap for shaft coverage offers a large amount of tissue with low donor site morbidity, avoiding unsightly scars in more visible parts of the body. The skin of the scrotum is the most similar to the skin of the shaft both for color, thickness, elasticity and consistency. Due to its pliability and extensibility during erection it provides satisfactory functional and cosmetic results. On the other hand the high density of hair of the scrotum represents a serious disadvantage and may require laser treatment removal. In conclusion we believe that the method we proposed works successfully representing a single stage procedure easy and safe to perform for like-for-like shaft reconstruction. This work is in line with the SCARE criteria [5].
A) Intra-operative view showing the dartos myo cutneous flaps harvested from the lateral part of the scrotum. B) The dartos myo cutneous flaps are rotated to cover the anterior surface of the shaft and sutured on the midline.
https://www.sciencedirect.com/science/article/pii/S2210261217302122
- 3
- 19
A 35-year-old male presented to the emergency department with bilateral forearm wounds. His past medical history was significant for untreated hepatitis C. He was unemployed and homeless. He reported injecting xylazine-laced fentanyl into his bilateral forearms. A physical exam revealed bilateral full-thickness skin wounds from the wrist to the proximal forearm over the ulnar border measuring [Figure 1]. The wounds appeared cavernous with undulated regions of eschar. Further, examination revealed exposed muscle and tendon bilaterally and some exposed muscle of the dorsal forearm compartments. His hand function was preserved.
The patient was admitted to the hospitalist and initiated on broad antibiotic treatment with intravenous vancomycin and piperacillin/tazobactam. His wounds were washed and covered at the bedside, and he underwent surgical debridement in the operating room the following day. Intraoperatively, the eschar layers were removed sharply with a knife until a bleeding surface was encountered. Exposed muscle layers were removed with a curette. The ulna had an intact periosteum. Large-volume irrigation was used to clean the wounds. A negative pressure wound therapy device was fitted to the bilateral forearms. The sponge was changed twice over six days. On a postoperative day seven, the patient was returned to the operating room. Granulation tissue was observed over the ulna, and the wounds appeared clean. The surgeon covered the area with a split-thickness skin graft taken from the thigh. A negative pressure wound dressing was placed over the skin graft. The patient left the hospital against medical advice (AMA) two days following the second surgery and did not follow up in the surgeon's office.
Approximately nine months later, the patient returned to the emergency room with a similar, smaller wound on the left forearm. On exam, both previous skin grafts had healed well, and the new wound was adjacent to the volar border of the skin graft and measured 8x4cm. The wound exhibited a cavernous appearance but did not have exposed muscle. The next day, surgical debridement was performed, followed by negative pressure wound therapy. The day after surgery, the patient left AMA with no follow-up reported since.
- 10
- 11
EDIT; They do this to relive pressure in the muscle and loss of circulation
- 1
- 3
- 3
- 21
A 54-year-old male arrived at the regional trauma center following a self-inflicted gunshot wound to the face (Figure 1).
The defect spanned the left side of the face inferolateral to the nose and inferior to the left eye. The defect had abraded and jagged edges. After stabilization, tracheostomy placement, and two rounds of debridement, a vascularized free fibula reconstruction was planned and performed using 3D modeling (Figure 2).
The intraoral defect was reconstructed using local tissues but dehisced following multiple attempts at intraoral closure. The initial closure attempts consisted of (1) local tissues at the time of initial flaps from the floor of the mouth and buccal lining tissue, followed by (2) spanning the defect with a thin piece of acellular dermal matrix (ADM) at a second operation, and (3) subsequently with another piece of ADM covered with a pedicled floor of mouth flap. These local flaps failed, exposing fibular bone and hardware. At the fourth operation, a split skin paddle STAIF was used for extra- and intra-oral coverage that led to stable coverage.
The design of the STAIF begins with identifying the superficial temporal artery (STA) via a Doppler probe. Typically, the STA is easily palpated approximately 2 cm anterior to the anterior helical rim and courses superiorly. In our experience, the flap may be elevated at least 5 cm past the last Doppler-able vessel location. After identifying the vascular course, the skin is pinched to visualize how much can be closed primarily. Marks are made to accommodate the primary closure of the donor site.
The skin paddle is incised and elevated in a superior to inferior direction. Additional temporoparietal (TP) fascia, galea, or pericranium may be included via undermining for more extensive coverage or fascial wrapping of the fibula or hardware. In this case, the TP, STA, and fascia were dissected down to the level of the temporalis muscle, keeping the pedicle with the flap. Dissection was maintained posterior to the course of the frontotemporal branch of the facial nerve, which lies immediately deep to the TP fascia. The skin paddle was islandized, and the flap elevated to the level of the zygomatic arch. A tunnel was made in the cheek superficial to the zygomatic arch at the level of the tragus. The flap was passed into the mouth, crossed the midline of the mandibular gingivobuccal sulcus, and sutured intraorally to cover the gingivobuccal sulcus of the lower lip and mucosal defect in the floor of the mouth (Figure 3).
For more extended reach, the flap may be passed under the zygomatic arch. In this case, the skin paddle was divided and split, providing both intra- and extra-oral coverage, like the methods described by Elbanoby et al. [3]. The distal skin paddle served for intraoral defect coverage; the proximal allowed for the reconstruction of the cheek and outer mouth after partial de-epithelization. The external facial defect was in the beard line and reconstructed with hair-bearing skin. The donor site was closed primarily after wide undermining and healed favorably. A Doppler signal was identifiable in each skin paddle.
Intraoral competence was restored following the STAIF use in this patient. Coverage of the fibula and hardware was obtained without further dehiscence or exposure (Figure 4).
He returned two months postoperatively for debulking and flap inset given an element of microstomia and difficulty with lip elevation. The flap was further divided at its tip into two portions for improved intra- and extraoral delineation and enhanced lip commissure definition. The split skin paddle STAIF successfully reconstructed intraoral defects and external cheek soft tissue wounds (Figures 5, 6).








 blop vorp
blop vorp 


















































 Slavshit
Slavshit

 Sandshit
Sandshit
